Most physicians are not in the habit of ordering hormone tests unless there is a problem (i.e., a woman is trying to get pregnant, etc.). But all women would benefit from hormone testing (along with other testing) as it provides great insight into the inner workings of the body.
I always recommend working with a clinician who understands the world of hormones. Hormones are complex, and although your OB/GYN may be the ideal health partner as you navigate the reproductive years, most OB/GYNs have had very little training on how to care for a woman during her perimenopausal and menopausal years unless they have specifically sought out this type of training. Many factors relating to food, lifestyle, and other considerations support optimal hormone balance. So, it’s critically important that women find a clinician who has had significant training in peri/menopause medicine.

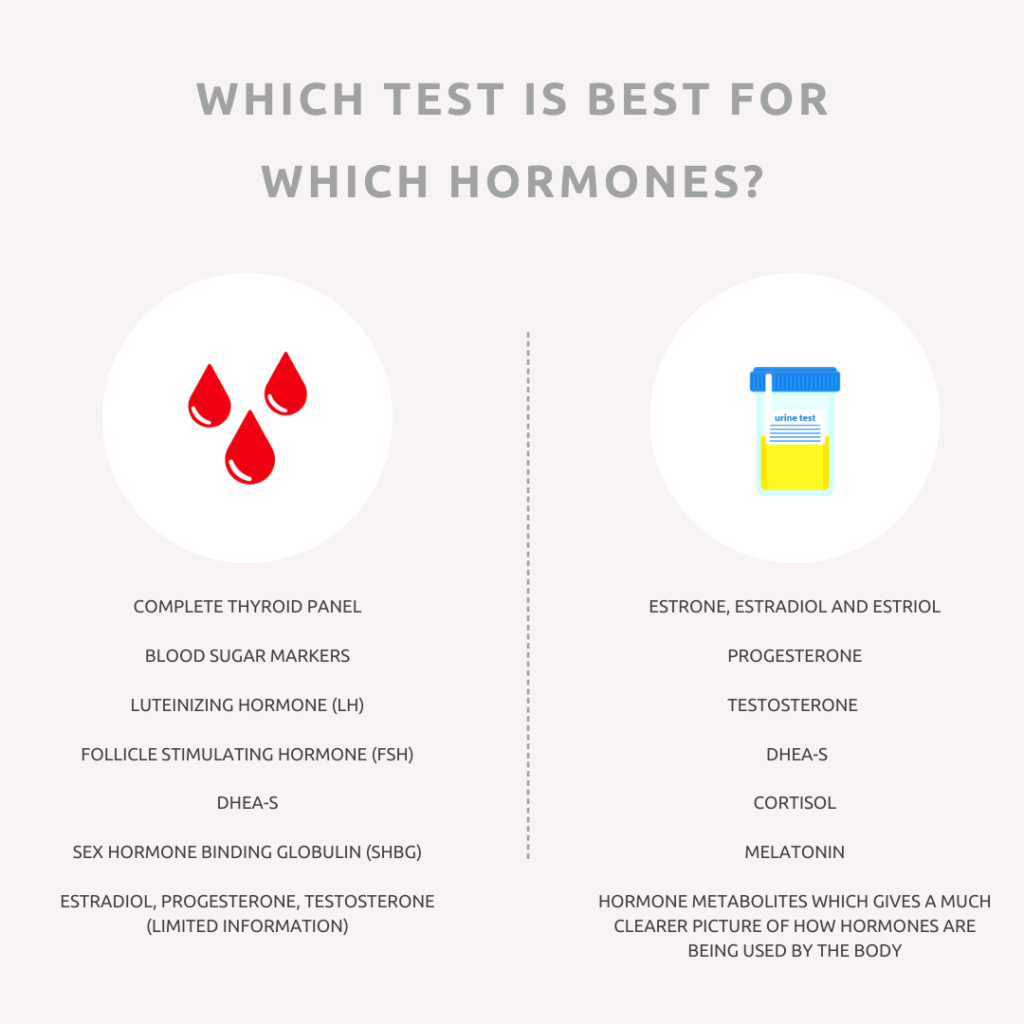
Different types of testing are critical to gaining an accurate hormone picture when it comes to testing. Let’s walk through each.
Blood Testing
Blood tests are also known as serum hormone tests, and they are the ones most commonly
ordered by your doctor. Blood tests can be used to check certain hormone levels accurately, but since hormone levels are constantly changing, a single blood draw only provides a snapshot of hormone levels at one point in time. This means it may not be the best option if you want to monitor changes in your hormone levels over a whole day, for example.
Overall, blood testing will give you a general picture of what is going on with your hormones. Timing is essential when measuring certain hormones such as estrogen, progesterone, follicle-stimulating hormone (FSH), and luteinizing hormone (LH). In a menstruating woman, estrogen levels begin to rise around day 3 of her menstrual cycle, peak around day 12 of her cycle, or just before ovulation, and then hit a second, more minor peak mid-luteal cycle (day 19-21, assuming a 28-day cycle), so it’s essential to test accordingly for the most accurate results. FSH and LH should be tested around day 3, along with estrogen levels.
Progesterone is barely detectable before ovulation and peaks 5-7 days after ovulation, so it must be measured mid-luteal cycle between days 19-21(assuming a 28-day cycle) to get accurate results. If a woman has irregular cycles because of hormone imbalances or perimenopause, serum testing may not be that accurate.
Blood testing is the only way to test thyroid hormones, blood sugar and metabolic markers, and other vital markers that provide insight into hormone function in the body.
An important note about hormone testing in pausal women
It’s important to note that women in their perimenopausal, menopausal, and postmenopausal years (and women who are in surgically induced menopause) have low levels of hormones. The technology used in traditional serum hormone tests may not accurately measure levels of serum hormones. You may wish to consider LC-MS/MS testing, which uses a specialized technology that is more accurate in detecting estrogen and testosterone levels in women with very low hormone levels.
Saliva Testing
Unlike blood-based tests, saliva tests can measure the amount of free, unbound hormone available to act on the target tissue. About 95-99% of steroid hormones circulating in the bloodstream are bound to carrier proteins. Saliva contains unbound, bioavailable hormones, which can give you a much clearer picture of how your hormones are functioning, especially if your total level of a particular hormone is low.
Because saliva tests can be taken multiple times throughout the day, they’re also helpful for measuring your daily free cortisol pattern (also known as your diurnal rhythm). Hormones are found in much lower concentrations in saliva than blood and urine, which can affect the accuracy of the results.
Saliva tests require patients to follow specific guidelines to collect an accurate sample. There are restrictions around eating, drinking, wearing lipstick, chewing gum, and teeth brushing that must be observed to get a usable specimen.
Saliva tests are also affected by topical and oral hormone usage. This means that if you’re using hormone supplements or hormone replacement therapy, saliva tests are not the best option for you. Like serum tests, the technology used in saliva testing does a very poor job of accurately measuring hormone levels in women with very low levels of hormones (i.e., women in menopause, post-menopause, surgically induced menopause, etc.).
One specific saliva test that I find very useful is the Cortisol Awakening Response When we wake up in the morning, cortisol levels naturally begin to rise by an average of 50%, so testing saliva cortisol levels 30 minutes after waking is an accurate way to capture the morning rise in cortisol. By 60 minutes after waking, cortisol levels have peaked and begun to decline. Measuring this rise and fall of cortisol levels at waking can be used as a “mini stress test” and can provide great insight into a person’s HPATG axis, which, affects all our hormones.
Urine Testing
24-hour urine hormone testing involves the collection of urine at several points throughout the day and night over 24 hours. Most 24-urine tests measure thirty or more hormones, including all three estrogens (estrone, estradiol, and estriol), progesterone, testosterone, and DHEA (a major precursor for sex hormones), adrenal hormones, and hormone metabolites, giving a much more comprehensive picture of how the body is using hormones. A growing body of evidence suggests that specific estrogen metabolites make a woman more prone to certain cancers and other diseases. These metabolites can only be measured in urine tests, which is why so many clinicians order these types of tests. Several companies offer urine hormone testing, including Rhein Labs, Genova, and Meridian Valley.
Testing estrogen and progesterone is not recommended in perimenopausal women
Estrogen and progesterone levels can fluctuate rather dramatically during perimenopause. This is especially true of estrogen, which can soar sky-high one moment and hit rock bottom the next as shown in the graph below.
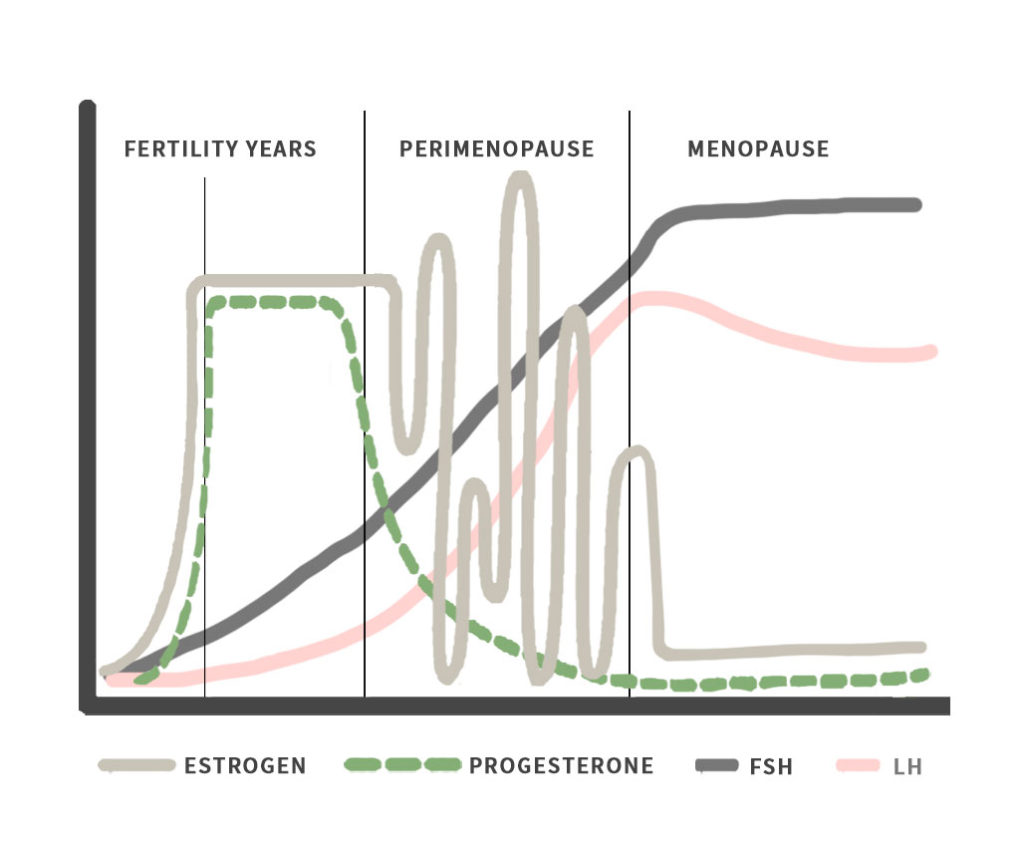
I have seen many practitioners deny women hormone replacement therapy and other supportive therapies/interventions simply based on an estrogen or progesterone level drawn at a single point in time.
For this reason, I generally do not recommend testing estrogen or progesterone during the perimenopausal years. Instead, track your symptoms which can provide great insight into the hormone changes that are happening in your body.
Optimal Ranges vs. Reference Ranges
Most doctors will interpret your labs using the reference range provided by the lab company. Many physicians and most patients do not understand that the reference range is not the same as the optimal range. The OPTIMAL RANGE describes the ideal or optimal result, meaning this is where your result should be for your body to function optimally.
The “reference range” for lab results is a set of values that includes a lab test’s upper and lower limits based on a group of people. Think of the reference range as simply telling you what 95% of the people at that lab had as a result. So, for instance, if all the women reading this article had their blood drawn, the reference range would reflect what 95% of us had as a result – so it’s more of an average of our collective results. Do you follow?
I find that most clients and patients understand this explanation for optimal ranges: If a passing grade at your kiddo’s school was 70% to 100%, would you prefer that your child earned 70%, or would you prefer a grade closer to 100%? Most parents would prefer a grade closer to 100% than the bottom of the grading scale. While 70% will make the cut to pass the class, a higher grade is ideal.
That’s a good analogy for interpreting labs using optimal ranges, often referred to as functional ranges. You want to know which levels are ideal or optimal for your body, not just the bare minimum needed to survive. When testing nutrient levels, a good rule of thumb is to be at least in the upper 1/3 of the reference range.
So, the next time you have labs done, ask your doctor to explain what your results mean and don’t assume that just because your result falls “within the reference range,” you are “good to go,” especially if you have symptoms. Clients often tell me that their doctor’s office left a voicemail saying their lab results were “normal.” Normal means average, and we don’t want to be average, considering that the average American is not that healthy. We want to ensure that our lab results fall within the optimal range. Make sense?
Lab work can be extremely helpful in helping to identify opportunities to prevent disease before it begins. You need to be sure that you are working with a practitioner who understands your labs and your symptoms and is willing to talk through the big picture with you.
One final note on hormone testing. Endocrine-disrupting chemicals (EDCs) play a huge role in disrupting our body’s ability to maintain hormone balance. The current hormone testing methods do not detect hormone-disrupting chemicals in the blood. If hormone levels are optimal, yet you continue to experience symptoms of hormonal imbalance, I would be highly suspicious that hormone-disrupting chemicals are to blame. It’s important to do what you can to reduce your exposure to EDCS and help your body get rid of excess toxins.
For more information on best practices regarding hormone testing, check out our discussion with Dr. Frank Nordt, Director & CEO of Rhein Labs. Dr. Nordt is an expert in hormone testing, and the replay of our discussion can be found in the Pausing Together Membership Community.
[i] Schofield, Ryan C., et al. “Data to Support a Simultaneous Testosterone and Estradiol Assay in Serum by LC-MS/MS.” Data in Brief, vol. 20, 2018, pp. 1160–1165., doi:10.1016/j.dib.2018.08.077.