One of my clients recently asked me if I thought she should stay on the pill until she hit menopause. My client is 43 years old and has been on the pill since delivering her last child, nearly eight years ago.

Her birth control history is much like that of many of my other clients. She was started on the pill in her teenage years for irregular periods, came off the pill to have babies, and then went back on the pill after having her last child.
When I asked her what prompted her to return to hormonal birth control after having her children, she said that her doctor recommended it. Her periods were irregular after the birth of her last child, and her doctor felt that the best way to “regulate” her periods was to stay on the pill “indefinitely” as he put it. “Just stay on the pill until you hit menopause, that way you won’t suffer perimenopausal symptoms,” he told her.
In my work with perimenopausal clients over the past several years, I’ve noticed that “the pill” has become the catch-all for any hormone-related imbalances.
Got crampy periods? Take the pill.
Miserable PMS? Take the pill.
Irregular periods? Take the pill.
Endometriosis? Take the pill.
Perimenopausal symptoms? Take the pill.
I too was treated with the pill back in my teenage years for irregular periods and miserable PMS. Had I known then what I know now, I never would have agreed to it.
While I’m not a fan of the birth control pill, I certainly support a woman’s decision to take the pill as long as she has been thoroughly educated about the pill’s impact on her body. But in my work with clients, I find that most women have no idea what the pill does to their body, especially as they enter the perimenopausal years, so I want to take some time now to share some insight.
Let’s start with a quick overview of hormones.
Here’s what you need to know about estrogen and progesterone.
Your two main sex hormones are estrogen and progesterone. Testosterone plays a role as well, but for today, we will focus mainly on estrogen and progesterone.
Contrary to what many women have been led to believe, hormones are not just for having babies. There are hormone receptors for estrogen and progesterone ALL over the body, not only in the reproductive organs! Hormones have a significant impact on the entire body from head to toe, and optimal levels are needed to support our brain health, heart health, skin health, immune health, reproductive health, and more.
I’d like you to think of estrogen and progesterone as lifelong partners. We need both in proper balance to keep the body functioning well. Too little, too much or the absence of either one and your body will suffer.
Estrogen is responsible for building the uterine lining in preparation for an implanted egg. But that’s not all: Estrogen keeps your brain in the game, supports healthy skin, plays a vital role in bone, heart and immune health and should be dominant in the first half of your menstrual cycle.
Progesterone is produced ONLY if a woman ovulates and its job (among other things) is to support and nourish a pregnancy. It should be dominant in the second half of your menstrual cycle. But that’s not all: Progesterone is a calming hormone, boosts thyroid hormone, reduces inflammation, promotes sleep, protects against heart disease, and prevents breast cancer.
Let’s take a look at the side-by-side comparison of these two hormones to get an understanding of what they do, why we need them and why they need to be in balance.
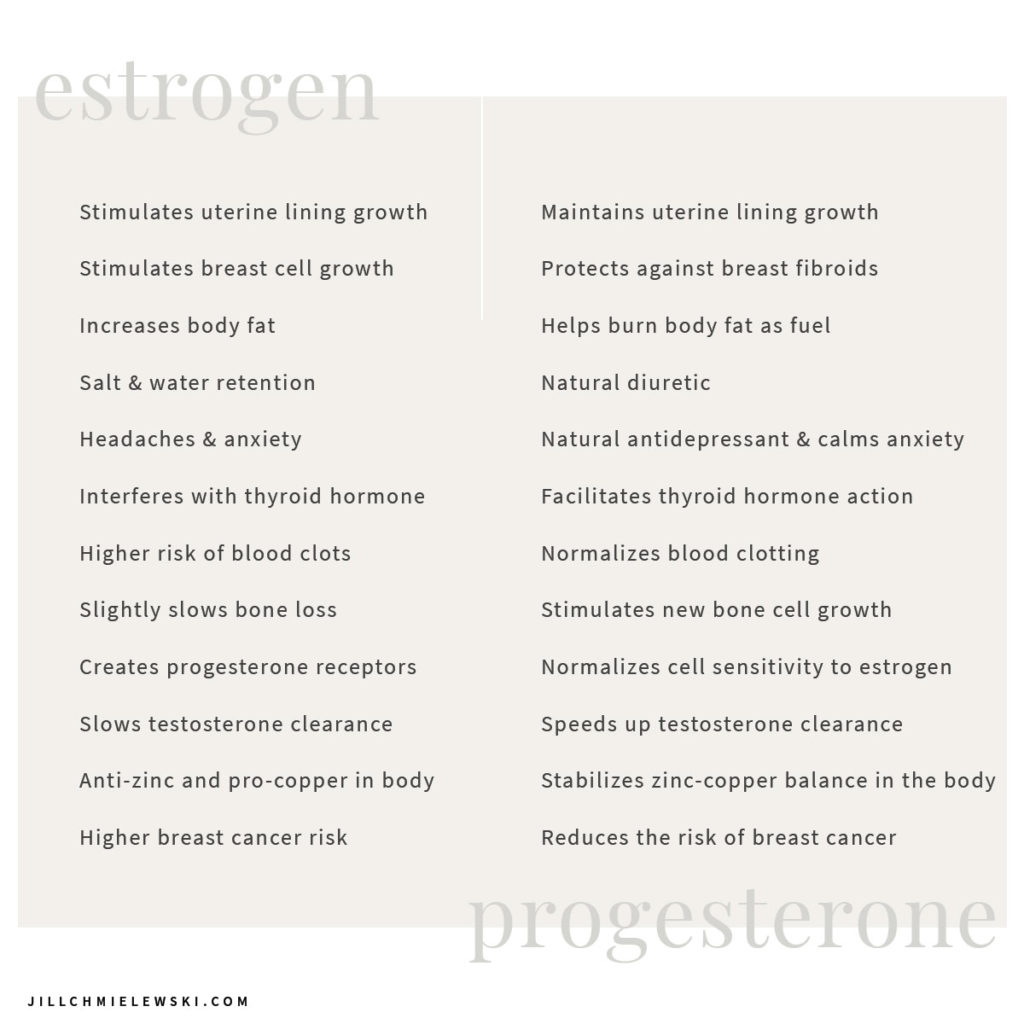
Estrogen and progesterone have very different functions in the body, and we need both for optimal health.
What happens when we go through perimenopause.
Perimenopause begins with a decline in progesterone, followed by a period of wildly fluctuating estrogen and ends with a decrease in estrogen. (For a deep dive into perimenopause, you can read my blog post “What is Perimenopause + What are the Most Common Symptoms of Perimenopause?”)
This decline in estrogen and progesterone results in many of the not-so-great symptoms of peri/menopause including low libido, vaginal dryness, dry, crepey skin, dry hair, sleep issues, low mood, low muscle tone, declining cognitive function, an increased risk for Alzheimer’s disease, increased risk for heart disease, osteoporosis, and more. It’s imperative that we hold on to every last drop of estrogen and progesterone during perimenopause so that we can reap the benefits of these amazing hormones for as long as possible.
Now, here’s what happens when you take the birth control pill.
Contrary to what your doctor may have told you, the birth control pill does not contain any estrogen or progesterone. That’s right. Instead, it contains synthetic chemicals such as ethinylestradiol, drospirenone, levonorgestrel (and others) that DO NOT have the same effect in your body that your sex hormones do. Their chemical structure is completely different! Please understand that these hormones are not identical to the hormones produced in your body, which means they do not offer the same benefits.
On top of adding synthetic chemicals to your body, the birth control pill works by suppressing your internal production of estrogen, and it inhibits ovulation, which means that you will not make progesterone either. Translation: While you are on the pill you are essentially in chemical menopause, and you will not reap the benefits that your sex hormones have to offer.
I recently attended the “Hack Your Cycle to Change Your Life” event in New York City, and Dr. Lara Briden referred to the effects of the birth control pill as “chemical castration”. And while that may sound a bit harsh, it’s an accurate reflection of the pill’s effect on your hormones. (I cannot imagine that there is a man on the planet who would voluntarily agree to be chemically castrated, can you??)
I don’t know about you, but I’d prefer to soak up every last bit of hormone benefit that I possibly can before my internal production of hormones declines.
The pill also causes nutrient deficiencies.
In addition to the fact that the pill suppresses all internal sex hormone production, it also ensures that a woman will suffer from nutrient deficiencies.
The most common deficiencies are:
Vitamin B6
Result: Depression, sleep issues, increased risk for heart disease, detoxification issues (especially estrogen detoxification)
Folate
Result: Birth defects, cervical dysplasia, anemia, increased risk for heart disease
Vitamin B1
Result: Depression, irritability, memory loss, muscle weakness, edema
Vitamin B2
Result: Problems with the skin, the eyes, the mucous membranes, and the nerves
Vitamin B3
Result: Cracked, scaly skin, diarrhea
Vitamin B12
Result: Anemia, depression, tiredness, weakness, increased risk for heart disease
Vitamin C
Result: Lowered immune system, easy bruising, poor wound healing
Magnesium
Result: Cardiovascular problems, asthma, osteoporosis, cramps, PMS, constipation
Selenium
Result: Lower immunity, reduced antioxidant protection, thyroid hormone conversion issues
Zinc
Results: Weak immunity, wound healing issues, issues with sense of smell/taste, sexual dysfunction
Since nutrients are the raw materials our body needs to function well, a nutrient deficiency of any kind is going to have a serious impact on the overall health of our body. And as we age, our ability to absorb nutrients declines, so the last thing we want to do is take a medication that all but ensures nutrient deficiencies.
Instead of the pill, what can you do to manage the symptoms of perimenopause?
It’s important to understand that it is normal and natural to experience hormonal changes during perimenopause. Much like puberty, when we went through some seriously rocky times, perimenopause can be a little tumultuous too, especially in the final few years before menopause. Periods can get longer, shorter, heavier, lighter, become more frequent or occur less frequently. That’s par for the course as your hormones go through the transition.
That said, there are things you can do to support your bod WITHOUT suppressing your internal hormone production. The specific support really depends on your symptoms and your hormone levels.
I always advise women to start with the basics ~ getting proper sleep and nutrition, managing stress, reducing toxins, carving out time for self-care and addressing the root causes of any ongoing imbalances are going to go a long way to help you as you go through this transition.
If you experience extremely heavy periods, clotty periods, or miserable PMS, you likely suffer from estrogen dominance, so you may want to check out my blog for helpful remedies. If you suffer from vaginal dryness, brain fog, mood changes or low libido, you are likely suffering from low estrogen, and you can read more about remedies here.
Every woman will have a unique perimenopausal experience, and it’s important to find a practitioner who deeply understands the role of hormones in the body and is willing to work with you to support your body through the perimenopausal years and beyond. If your doctor’s only solution for perimenopausal symptoms is the birth control pill, it’s time to find a new doctor.
References:
https://www.larabriden.com/the-pill-is-bad-medicine-7-ways-that-hormonal-contraception-harms-women/
https://www.ncbi.nlm.nih.gov/pubmed/21967158
https://experiencelife.com/article/hormonal-birth-control-aviva-romm/
Tassone, Shawn. Contraception Deception: Open and Honest Discussion about Birth Control Between Your. Emmaus Road Publishing, 2018.